Abstract
Introduction:
Sepsis is a life-threatening condition in which the host's response to a systemic infection contributes significantly to mortality. Patients with sepsis are at risk of developing a coagulation disorder leading to disseminated intravascular coagulation (DIC). In DIC, widespread activation of the coagulation cascade leads to microvascular thrombosis and organ failure. This consumes platelets and coagulation factors, putting the patient at risk for bleeding. Cortisol is a steroid hormone released in response to stress. Cortisol levels have been found to be increased in sepsis patients, and high cortisol levels have been correlated with increased mortality. However, the association of cortisol levels with the severity of coagulopathy in patients with DIC remains unclear. Cortisol levels may also be relevant to disease progression as a link between the stress response and the immune system. The purpose of this project is to assess the association of plasma cortisol levels with severity of coagulopathy in a population of patients with sepsis and clinically confirmed DIC. Furthermore, the association of cortisol with markers of hemostatic status, inflammation, and platelet function were also assessed.
Materials and Methods:
Citrated, de-identified plasma samples were collected from 52 adults with sepsis and suspected DIC at the time of ICU admission. Samples were collected at the University of Utah and transferred to Loyola
University Chicago under an IRB approved protocol. Plasma samples from healthy individuals were acquired from a commercial source (George King Biomedical, Overland, KS). Samples were stored at -80˚C prior to analysis. Platelet count was determined as part of standard clinical practice. PT/INR and fibrinogen were measured using standard techniques on the ACL-ELITE coagulation analyzer. Cortisol, D-dimer, PAI-1, CD40L, inflammasomes (NLRP3), and microparticles were measured using commercially available ELISA kits and were performed according to the manufacturer's instructions. DIC score was calculated using the ISTH scoring algorithm. A score of 0-2 was classified as no DIC, 3-4 was classified as non-overt DIC, and 5 or greater was classified as overt DIC. Results were analyzed using GraphPad Prism.
Results:
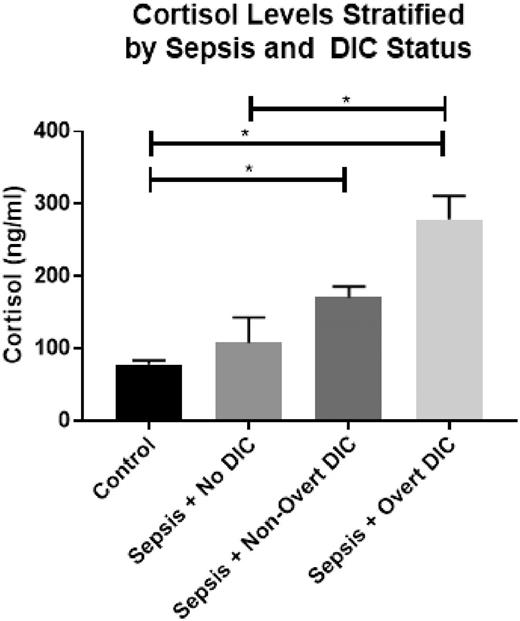
Cortisol showed significant variation based on DIC status (Kruskal-Wallis ANOVA, p < 0.0001) . Patients with non-overt DIC and overt DIC exhibited significantly elevated cortisol levels compared to healthy controls (p < 0.0001 for both groups). Furthermore, cortisol levels showed significant variation amongst sepsis patients based on DIC score. Patients with sepsis and overt DIC had elevated cortisol compared to patients with sepsis and no DIC (p = 0.0069). Data is shown in Figure 1.
Correlations were evaluated between cortisol and the hemostatic markers platelets, fibrinogen, INR, D-Dimer, and PAI-1 as well as with the inflammatory marker, inflammasomes (NLRP3) and the platelet markers CD40L and microparticles. Cortisol showed significant correlations with D-Dimer, PAI-1, and INR. (D-Dimer Spearman r = 0.480, p = 0.001; PAI-1 Spearman r = 0.415, p = 0.002; INR Spearman r = 0.305, p = 0.037). No significant correlations were observed between cortisol and the markers of inflammation or platelet activation.
Conclusions:
Cortisol showed a significant association with hemostatic status in a population of patients with sepsis and well-defined coagulopathy. Cortisol levels were significantly elevated in patients with overt or non-overt DIC compared to healthy individuals and in patients with overt DIC compared to those with sepsis without DIC. Cortisol also showed significant correlations with markers of hemostatic activation but not with markers of inflammation and platelet activation. This suggests that elevated levels of cortisol may play a specific role in the progression of hemostatic dysregulation observed in sepsis and DIC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal